Ablation d’une fibrillation atriale
Cette technique repose sur l’exclusion/isolation des foyers initiateurs à l’origine de certaines FA paroxystiques.
Plusieurs techniques existent (cf. Ablation)
La technique classique est longue et difficile, réservée aux centres spécialisés (pour une isolation des 4 veines pulmonaires par cryoablation, il faut réaliser un cathétérisme trans septal pour positionner les sondes dans l’oreillette gauche puis dans les quatre veines pulmonaires, une par une) (Cf. Ablation d’une FA : technique).
L’ablation par électroporation est appelée à supplanter la technique classique [11]
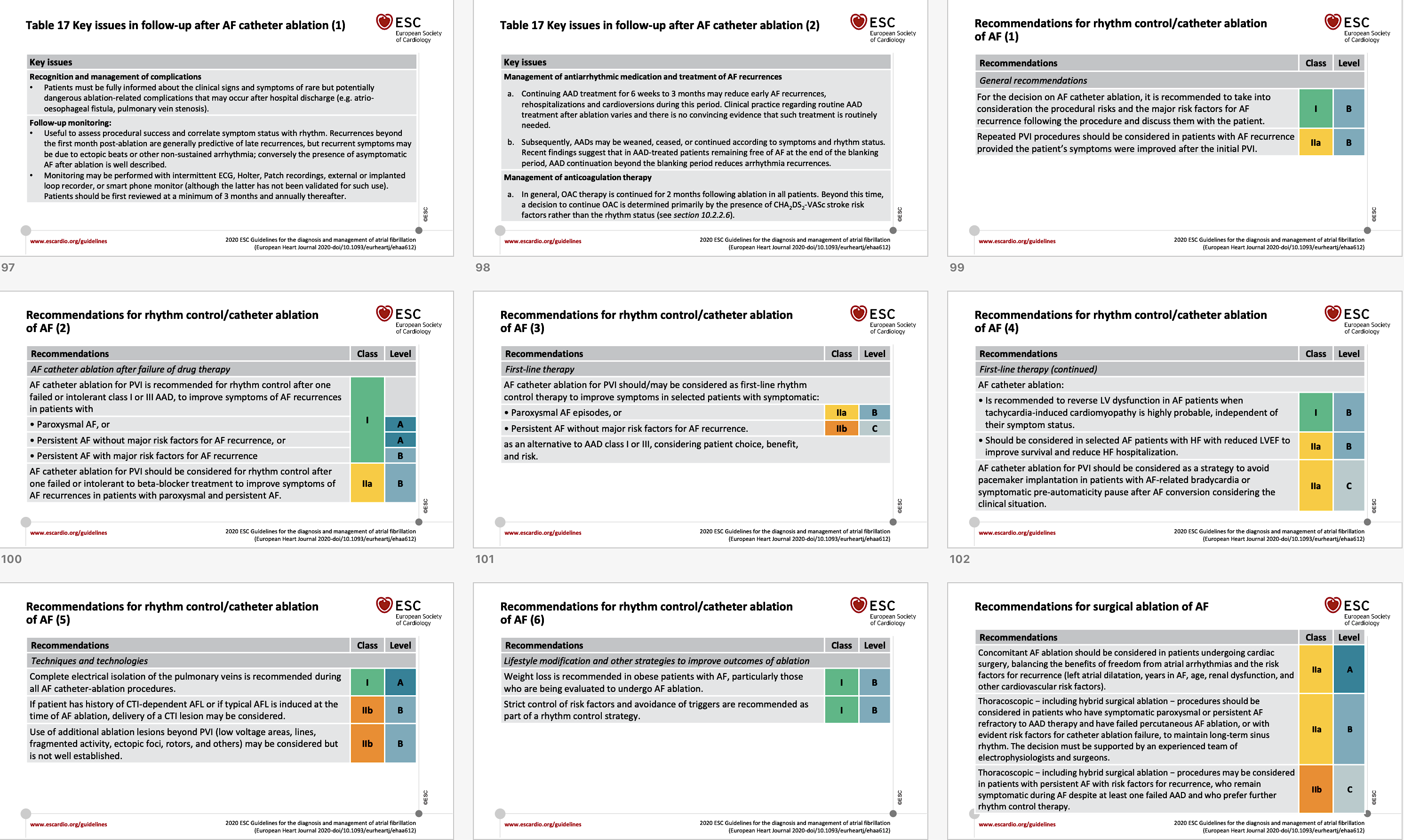
Référence ESC 2020 (voir diapositives 94-102) [1]
The European Society of Cardiology Guidelines for the diagnosis and management of AF recommend (Class IA) rhythm control therapy for symptom and quality of life improvement in symptomatic patients with AF.
For rhythm control, catheter ablation is a Class IIA recommendation, according to the patient choice, which raises to Class IA in AF patients with heart failure with reduced ejection fraction and for failed drug therapy.
Version résumée française (indications)
- FA paroxystique récidivante et symptomatique sous antiarythmiques (IA) ou en première intention chez des patients sélectionnés et symptomatiques selon leur choix (IIA).
- FA symptomatique pour une insuffisance cardiaque avec FEVG altérée possiblement rythmique (pour améliorer les symptômes et la FEVG) (IA) –> voir cardiomyopathie rythmique
- FA persistante réfractaire aux antiarythmiques (pour améliorer les symptômes (IIA)
- Pour éviter l’implantation de stimulateur si bradycardie liée à la FA (IIA)
Efficacité
- L’ablation initiée précocement après la révélation du diagnostic (< 1 an en général) offre une prévention plus efficace des récidives de FA que le traitement antiarythmique [1][2]. L’ablation (« pulmonary vein isolation with cryoballoon« ) est statistiquement plus efficace qu’un traitement antiarythmique (classe I ou III) en premier intention d’une FA paroxystique chez des sujets relativement jeunes, mais le bénéfice est modeste à un an [8].
- Elle améliore la qualité de vie des formes symptomatiques [3][4] et des insuffisants cardiaques [10].
- Elle réduit le risque de récidives de FA (rémission > guérison), de façon variable selon l’ancienneté de la FA (meilleure si plutôt paroxystique que persistante ou si ancienneté < 2 ans), le nombre de procédures réalisées (souvent deux à trois), la correction des facteurs de risque associés (surcharge pondérale, apnée du sommeil…), l’adjonction d’un traitement antiarythmique, et surtout la durée et la méthode de surveillance des récidives [3][5][6][7]….
- Elle n’améliore pas la survie ni le nombre d’accidents vasculaires cérébraux [3][10].
- Elle ne dispense pas d’une anticoagulation au long cours dans la majorité des cas.
- La question de savoir si la cryoablation peut être proposée comme traitement de première intention pour certains patients atteints de FA remplaçant les médicaments antiarythmiques mérite confirmation en 2022 [9].
Biblio commentée (réservée aux abonnés)
La suite est réservée aux membres et stagiaires du site.
Se connecter | Devenir membre | Devenir stagiaire
